Gastric Sleeve Abroad: Lithuania
We are one of the leading bariatric surgery clinics for medical tourists in the European Union. We are proud of the fact that over 90 % of our patients come from the UK, Ireland, Norway, Sweden, Denmark, Germany, Switzerland and other countries.
See before-after pictures
Reviews and Facebook group
Our patients and clinic in the media
Prices
- Gastric sleeve – 5.450 £
- Hiatal hernia repaired during weight loss surgery for FREE.
- Plastic surgery after a massive weight loss – from 580 £
Regular consultations with Prof. Almantas Maleckas in London
- accommodation with medical care – from 62 £ per night
- plastic surgeon consultation 12 months after surgery (if interested) – FREE
Regular price:
- consultation with the surgeon and anaesthesiologist
- all the necessary health tests before and after the surgery
- bariatric surgery
- anaesthesia
- hospital stay (1-3 days) with 24 hours medical care
- 24/7 personal assistance during your stay
- transfers to / from the airport, hotel and clinic
- diet instructions after bariatric surgery
- FREE dietician follow-up for 5 years
Get your surgery for free by claiming a refund from your local health board. We cooperate with HSE and other health boards across the EU to help our Irish and EU patients receive a refund for their weight loss surgery in Lithuania. The clinic helps with the documents needed to claim a refund after following the EU directive route for medical treatment abroad.
Please note that the price of the surgery itself is provisional and may be accurately assessed only after the evaluation of each individual case.
The default currency at our clinic is EUR, so if you were looking at prices in GBP it may vary depending on GBP / EUR exchange rate at the moment of payment.
Things to consider when choosing a clinic and surgeon abroad:
- Is it a World-class surgeon with similar experience to ours (700 bariatric surgeries per year) ?
- Is bariatric staff available? We are one of the few clinics that has a specially trained bariatric nursing staff.
- Experience with bariatric anaesthesia? Anaesthesia of overweight patients requires skill and specialised experience, and our anesthesiologists have been specialising in bariatrics for over 15 years.
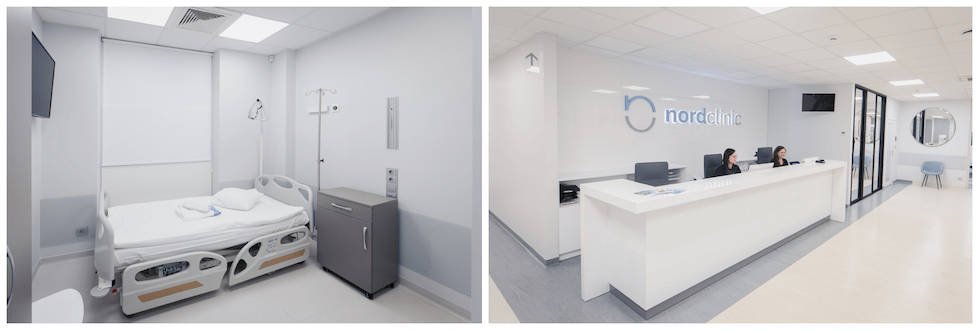
- Is it a multidisciplinary private hospital? Nordbariatric is a private clinic with modern facilities and exceptional care.
- Overall knowledge in the field? We have designed a unique bariatric mobile app. Our surgeon is the co-author of more than 40 scientific articles.
All of our patients can use one of our offers available at the moment.
- Additional services in our clinic. You or your accompanying persons can explore the various services by following this link. Customise your preferences and request to book any preferred procedures.
- Brand ambassador discount. If you have a community that would be interested in our services, you can now get a discount for your procedure by spreading the word about our clinic on your social media. Contact your customer service representative for more information.
- Recommendation discount. Get a discount for your next plastic or gynaecology procedure by recommending our clinic. Contact your customer service representative for more information.
- Gastric sleeve – 6.150 €
- Hiatal hernia repaired during weight loss surgery for FREE.
- Plastic surgery after a massive weight loss – from 700 €
Regular consultations with Prof. Almantas Maleckas in London
- accommodation with medical care – from 74 € per night
- plastic surgeon consultation 12 months after surgery (if interested) – FREE
Regular price:
- consultation with the surgeon and anaesthesiologist
- all the necessary health tests before and after the surgery
- bariatric surgery
- anaesthesia
- hospital stay (1-3 days) with 24 hours medical care
- 24/7 personal assistance during your stay
- transfers to / from the airport, hotel and clinic
- diet instructions after bariatric surgery
- FREE dietician follow-up for 5 years
Get your surgery for free by claiming a refund from your local health board. We cooperate with HSE and other health boards across the EU to help our Irish and EU patients receive a refund for their weight loss surgery in Lithuania. The clinic helps with the documents needed to claim a refund after following the EU directive route for medical treatment abroad.
Please note that the price of the surgery itself is provisional and may be accurately assessed only after the evaluation of each individual case.
The default currency at our clinic is EUR, so if you were looking at prices in GBP it may vary depending on GBP / EUR exchange rate at the moment of payment.
Things to consider when choosing a clinic and surgeon abroad:
- Is it a World-class surgeon with similar experience to ours (700 bariatric surgeries per year) ?
- Is bariatric staff available? We are one of the few clinics that has a specially trained bariatric nursing staff.
- Experience with bariatric anaesthesia? Anaesthesia of overweight patients requires skill and specialised experience, and our anesthesiologists have been specialising in bariatrics for over 15 years.
- Is it a multidisciplinary private hospital? Nordbariatric is a private clinic with modern facilities and exceptional care.
- Overall knowledge in the field? We have designed a unique bariatric mobile app. Our surgeon is the co-author of more than 40 scientific articles.
All of our patients can use one of our offers available at the moment.
- Additional services in our clinic. You or your accompanying persons can explore the various services by following this link. Customise your preferences and request to book any preferred procedures.
- Brand ambassador discount. If you have a community that would be interested in our services, you can now get a discount for your procedure by spreading the word about our clinic on your social media. Contact your customer service representative for more information.
- Recommendation discount. Get a discount for your next plastic or gynaecology procedure by recommending our clinic. Contact your customer service representative for more information.
Patient stories
Only we can offer:
One of the most experienced private bariatric clinic teams in Europe. More than 7.000 bariatric surgeries were performed by our surgeon to this date. A figure that no surgeon or clinic in a region can match.
The only clinic in Europe with a specially designed bariatric mobile app for patients after weight loss surgeries. Available in 6 languages on iOS as well as Android devices.
Watch Peter's gastric bypass story
Refund for EU patients

Get your surgery for free by claiming a refund from your local health board. The clinic helps patients with the documents needed to claim a refund after following the EU directive route for medical treatment abroad. It applies to patients who are insured under the systems of one of the EU countries and may not get the surgery due to long waiting times. On average our patients from the EU countries get fully refunded by their local health board in 3-5 months after their surgeries.
Bariatric Team

- Our surgeon Almantas Maleckas is a doctor of medical science
- UK General Medical Council (GMC) certified
- He performed over 7.000 bariatric operations
- A pioneer in laparoscopic surgery in the region
- More than 15 years working experience in Sweden, Gothenburg University hospital
- Works both in Lithuania and Sweden, speaks fluent English and Swedish
- London School of Economics graduate

- Our surgeon Nerijus Kaselis is a doctor with a degree in medicine
- Member of the International Federation of Obesity
- Has been practising abdominal surgery for over 32 years, specialising in bariatric surgery for the past 18 years
- Was the first surgeon to perform various laparoscopic surgeries in Lithuania
- Works as a team lead of surgeons in complicated obesity surgeries abroad
- Has international work and study experience

- Our surgeon Linas Venclauskas has over 15 years of experience
- Specialises in minimally invasive surgery, surgical treatment of the upper gastrointestinal tract and bariatric surgery
- Associate Professor at Lithuanian University of Health Sciences
- President of the Kaunas Society of Surgeons
- A member of the European Hernia Society
- Chairman of the Lithuanian Society of Hernia Surgery

- Our surgeon Aurika Karbonskiene has over 25 years of experience as anesthesiologist
- Over 15 years of experience as a bariatric anesthesiologist
- Since 2008 – Associate Professor at Lithuanian University of Health Sciences
- Board member of Lithuanian Society of Anesthesiologists and Intensive Care Physicians
- Member of the European Society of Anesthesiology
- Researcher and coordinator at the Clinical Trial Network of European Society of Anesthesiology

- Our surgeon Almantas Maleckas is a doctor of medical science
- UK General Medical Council (GMC) certified
- He performed over 7.000 bariatric operations
- A pioneer in laparoscopic surgery in the region
- More than 15 years working experience in Sweden, Gothenburg University hospital
- Works both in Lithuania and Sweden, speaks fluent English and Swedish
- London School of Economics graduate

- Our surgeon Nerijus Kaselis is a doctor with a degree in medicine
- Member of the International Federation of Obesity
- Has been practising abdominal surgery for over 32 years, specialising in bariatric surgery for the past 18 years
- Was the first surgeon to perform various laparoscopic surgeries in Lithuania
- Works as a team lead of surgeons in complicated obesity surgeries abroad
- Has international work and study experience

- Our surgeon Linas Venclauskas has over 15 years of experience
- Specialises in minimally invasive surgery, surgical treatment of the upper gastrointestinal tract and bariatric surgery
- Associate Professor at Lithuanian University of Health Sciences
- President of the Kaunas Society of Surgeons
- A member of the European Hernia Society
- Chairman of the Lithuanian Society of Hernia Surgery

- Our surgeon Aurika Karbonskiene has over 25 years of experience as anesthesiologist
- Over 15 years of experience as a bariatric anesthesiologist
- Since 2008 – Associate Professor at Lithuanian University of Health Sciences
- Board member of Lithuanian Society of Anesthesiologists and Intensive Care Physicians
- Member of the European Society of Anesthesiology
- Researcher and coordinator at the Clinical Trial Network of European Society of Anesthesiology
5-year follow up with dietitian
Nutrition is one of the main focus after weight loss surgery to maximize weight loss and prevent weight gain. We offer a dietitian who will talk with you about the diet you’ll need to follow after surgery, explaining what types of food and how much you can eat at each meal. Karolina is a dietitian and Nutrition Consultant with a degree in the medical field. Read more about her here.
11 reasons that make us the most popular bariatric clinic abroad
Our team of 3 bariatric surgeons has 15-20 years of experience in the field in total performing over 500 different bariatric surgeries per year. Moreover, our surgeons are members of various prestigious surgical societies both Lithuanian and international. Our leading bariatric surgeon Dr Almantas Maleckas has performed more than 7.000 bariatric surgeries. He is fluent in four languages, among which English and Swedish. The surgeon has been regularly working in Sweden for over 15 years. Dr Maleckas is a pioneer of laparoscopic surgery in Eastern Europe and has trained many other bariatric surgeons in the region.
We are one of the leading bariatric surgery clinics for medical tourists in the European Union. We are proud of the fact that over 90 % of our patients come from the UK, Ireland, Norway, Sweden, Denmark, Germany, Switzerland and other countries.
We are trusted by our patients and we appreciate all the reviews and feedback collected over the years. Find testimonials here or on Google.
Already more than 5.000 of our former, current and future patients joined our online community with the aim to build a space for opinions and mutual support. Members are welcome to share experiences about their visit to the clinic and to discuss all surgery-related matters.
We offer a 5-year follow-up which includes being able to get in touch with our Lithuanian dietitian Karolina. She is consulting patients after surgery and is available upon request to answer postoperative nutritional questions for five years after surgery.
Our clinic is the only clinic that has developed its own app designed specifically for bariatric patients – Bariatric IQ. The most useful feature of this app is special bariatric diet recommendations based on a particular product, a patient’s gender, time after surgery and other factors. Such a feature has not been replicated by any other bariatric apps in the world. Read more and download the app on your IOS or Android smartphone here.
Our clinic works according to the highest standards set by the European Union. This helps to guarantee the quality of medical services. We care about the safety, comfort and successful results of our patients from all over the world.
The clinic helps patients with the documents needed to claim a refund after following the EU directive route for medical treatment abroad. It applies to patients who are insured under the systems of one of the EU countries and may not get the surgery due to long waiting times.
We provide customer service in 9 foreign languages including English, Swedish, Norwegian, Danish, Italian, Spanish, French, Russian, Polish. Everyone in our clinic speaks English, including nurses, assistants and the surgeon.
Combining different plastic surgery procedures to offer optimal treatment for post-bariatric patients has been our plastic surgery department’s specialisation for many years now. We have performed such surgeries for more than 10.000 patients to this date. Since weight loss patients often require multiple surgical procedures to address excess skin, surgery planning and surgeons’ experience are very important. We carefully select patients, evaluate each case individually, and only agree to combine surgeries within health & safety limits. Our team of 9 plastic surgeons performs more than 3.000 plastic operations a year, a number that no other clinic in Central & Eastern Europe can match.
Special bariatric app for your mobile phone
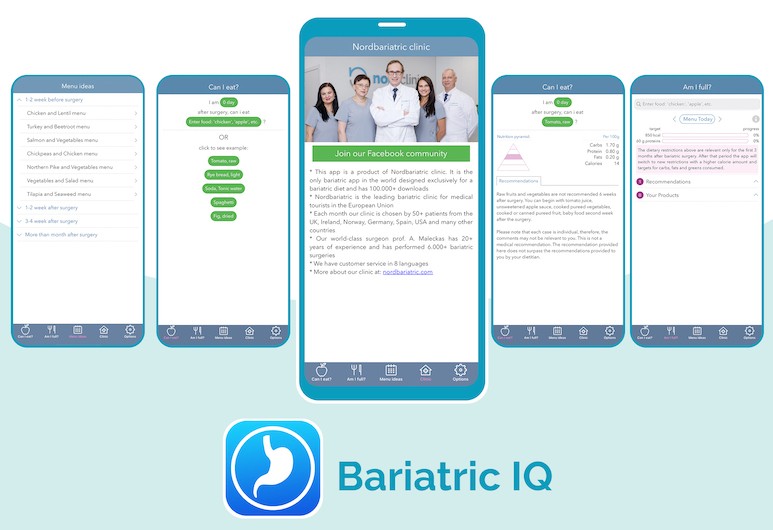
- Created by Nordbariatric clinic
- Special bariatric diet recommendations based on a particular product, a patient’s gender, time after surgery and other factors
- Available in 6 languages
- Available on iOS as well as Android.
- To this date the app was downloaded more than 100.000 times!
- Read more
Direct flights to Lithuania







Our clinic

Self-catered accommodation with medical care
What is a gastric sleeve? The history of gastric sleeve surgery.
Gastric sleeve surgery, or a laparoscopic sleeve gastrectomy, is a surgical procedure during which a part of the stomach is removed leaving the remaining part to function as a new smaller stomach. The stomach is an organ which functions as a temporary food reservoir and it also produces hormones, such as gastrin and ghrelin. Ghrelin is associated with the feeling of hunger. Therefore, the removal of a large portion of the pouch can favorably alter the hunger hormone production. After a gastric sleeve procedure a patient’s food intake is decreased and they feel full faster. It is a bariatric surgery, which helps patients to lose as much as 50 to 70 percent of their excess weight.
The history of gastric sleeve surgery might be described as an evolutionary process of prior anti-reflux surgery and gastroplasty. The first duodenal switch was performed in 1988 and it later evolved to an open gastric sleeve surgery. In 1999 the first laparoscopic gastric sleeve surgery was performed, meaning that surgeons no longer had to perform open surgeries and instead patients could be operated by making just a few incisions in the abdomen as it is mostly practiced today.
FAQ sessions with our surgeon
Watch full list of interview sessions on our Youtube channel.
How is gastric sleeve performed?
Gastric sleeve surgery is performed under general anaesthesia and takes about two hours to complete. Just a few small incisions are made in the stomach area so that a laparoscope and other surgical instruments used to perform a gastrectomy can be inserted in the abdomen. Then approximately 75 percent of a stomach is removed and the rest of the pouch is sealed using medical staples. In order to prevent any leakage after a patient starts consuming food, the staples are then manually stitched over and a fluid test is done while the patient is still on the operating table. The new stomach acquires a shape somewhat similar to a sleeve. The stomach retains all of its previous functions, therefore, food can still be digested properly. The biggest change is a significantly decreased feeling of hunger. Moreover, the patient feels full faster and can eat smaller portions of food.
Who is a good candidate for gastric sleeve?
Not every obese person can qualify for a gastric sleeve surgery. A qualified physician will help to determine if a patient is eligible for the procedure. However, there are certain requirements that must be fulfilled so that the patient can be approved for the surgery.
A suitable candidate for a gastric sleeve surgery is someone who tried losing weight individually through a healthy diet and exercise but found it ineffective. A patient should have a body mass index (BMI) of 35 or more. A BMI of 30 to 35 is considered sufficient for undergoing gastric sleeve surgery if a patient is present with additional medical conditions related to obesity, such as type 2 diabetes or arterial hypertension.
Bear in mind that surgery results greatly depend on a patient’s commitment to stick to a new routine and strictly follow doctor’s recommendations for a successful recovery. The right attitude towards physiological and psychological health is also undeniably important.
How is sleeve different from bypass?
There are a number of possible procedures bariatric patients can choose from. Although gastric sleeve and gastric bypass procedures are similar in recovery time, possible risks and weight loss results their surgical methods differ.
After a gastric sleeve surgery as well as after a gastric bypass a patient needs approximately 2-4 weeks to recover.
Both surgeries have a chance of provoking a dumping syndrome, which is caused by the food passing through the stomach and reaching the small intestine too quickly.
On the other hand, both surgeries are very effective in achieving long-term weight loss. They can both help a patient lose more than 60 percent of their body weight in the first year after the surgery.
During a gastric sleeve surgery a surgeon removes a part of the stomach and then seals it with a titanium staple line as well as a manual stitch that prevents bleeding and leakage. During a bypass surgery stomach is divided into a small upper pouch and a large “remnant”. The smaller pouch functions as a new stomach just a significantly smaller one. Then the middle part of the small intestine is attached to that small pouch creating a bypass. When the food travels through the digestive system it bypasses most of the stomach and the first part of the small intestine, therefore, a smaller amount of food is consumed and fewer calories are obtained.
During a consultation the surgeon will evaluate each case, discuss available options and choose the procedure that best fits the patient’s needs.
The benefits of gastric sleeve surgery
- Gastric sleeve surgery is a life-changing procedure which allows a patient to lose more than 60 percent of their excess body weight.
- Studies prove that a significant reduction in one‘s weight causes a remission of serious health-damaging conditions, such as arterial hypertension, diabetes, sleep apnea, heart failure, osteoarthritis and back pain.
- Moreover, patients also report having more vitality and energy to engage in new physical activities.
Is gastric sleeve reversible?
During a gastric sleeve surgery three-quarters of the stomach are removed and the remaining pouch is shaped into a sleeve-like shape. Due to the extent of surgical invasion gastric sleeve cannot be reversed. The volume of the stomach pouch is reduced permanently therefore the production of hunger hormone decreases accordingly. This ensures consumption of small portions of food for the rest of one’s life, which means that weight loss will be reliable and permanent just as the surgery.
How to prepare for gastric sleeve surgery? What tests are needed?
Weight loss surgery is a life-altering decision to make, therefore, a patient should be prepared psychologically as well. The treatment does not start and end with just the surgery and is rather a choice of a new way of life. Therefore, patients need to be aware of numerous lifestyle alterations which are essential for successful recovery and life-long results.
At first, the prospective patient should consult a general practitioner who will evaluate the patient’s eligibility and emotional well-being. This is an important step since obesity might result from stress or binge eating which have other treatment methods.
Bear in mind that the preparation process might start as early as a year before the surgery so that the patients lose at least 5-10 percent of their body weight. The medical team including a bariatric physician, a dietologist and a psychologist will put together a treatment plan and will follow-up with the patient during the pre-surgery period. Adopting healthy habits ensures a stable weight loss and a successful recovery period.
A patient must refrain from smoking 8 weeks before surgery and preferably quit smoking altogether after surgery, as smoking increases the risk of complications by restricting the blood flow.
Also, consumption of some medications, especially blood-thinning drugs, should be discussed with the doctor a couple of weeks before the procedure.
Certain laboratory tests such as complete blood count are performed before the surgery. An electrocardiogram and a gastroscopy are also needed for an accurate assessment. In individual cases, the surgeon might suggest additional tests to be carried out as well.
Two weeks before the surgery a patient will have to stick to a certain diet and calorie goal. The main purpose of the pre-surgery diet is to shrink the patient’s liver in size by losing the fat around it so that it is easier for a surgeon to access the near lying stomach. In order to prevent regurgitation, the patient must not eat anything 6 hours before the procedure.
What are the risks of gastric sleeve surgery?
The risk of complications can be reduced by choosing a well-experienced doctor and strictly following a treatment plan. Moreover, the risk is reduced significantly if a patient does not smoke and is eager to commit to a healthy lifestyle. The possible complications are:
Acid reflux can develop as a result of a reduced stomach size when gastric juice leaks into oesophagus and damages the mucosal layer. Therefore, antacid medication is recommended at least the first 3 months after surgery.
Staple line leaks may occur if the body fails to form a complete seal over the staple line which was used during the surgery to close the reduced stomach. However, stitching over the staple line reduces the risk of leakage to an absolute minimum.
Blood clots can form during general anaesthesia or during recovery period because blood moves more slowly through the veins than usual. In order to prevent blood clots a patient should start walking as soon as possible and refrain from smoking.
Dumping syndrome occurs when food reaches small intestine too quickly. An early dumping syndrome is caused by a sudden influx of food which subsequently makes fluids from the bloodstream rush into intestines. This causes diarrhea and bloating. A secondary dumping syndrome is caused by starches breaking down too fast and causing sudden fluctuations in blood sugar level. Dumping syndrome can be avoided by adjusting portion sizes and choosing products carefully and trying each new product slowly and in small quantities.
What to expect after gastric sleeve surgery?
- After gastric sleeve surgery a patient should expect to spend at least a few days at the hospital.
- At first the patient will have intravenous pain relieving medications administered. When discharged from the hospital patient will be prescribed pain-relieving drugs to be taken at home.
- The patients should wait 48 hours until having a shower and should avoid baths, pools and hot tubs for four weeks or until the wounds have healed completely and are dry. The patient will be advised on a more detailed wound care by the healthcare team.
- The patient should expect to return to usual activities in about 2 to 4 weeks, but refrain from sports and strenuous training for 2 months. In order to ensure stable weight loss regular exercise, like swimming or walking, should gradually become a part of one’s life.
- A specific diet will also have to be followed, which will be discussed in the next paragraph.
What will I be able to eat after gastric sleeve surgery?
Right after the surgery a patient should consume only clear liquids. Sugar should be avoided as it may contribute to a dumping syndrome, which is caused by a rapid influx of sugars. Coffee may worsen acid reflux and thus should be limited to a minimum as well. Carbonated drinks should not be consumed as they cause gas formation. While still at the clinic, the patient will be introduced to pureed food and low-fat yoghurt. Pureed diet is advised for approximately six weeks after surgery.
During this period the patient is advised to consume baby food or homemade vegetable and lean meat purees, low-fat yoghurt without chunks, protein shakes, homemade clear broth. Baked and pureed apples, peaches or pears may be introduced as a snack, but preferably consumed in the first part of the day, as fruit are high in sugars. If not enough proteins are consumed with foods, protein powder may be added to the purees. Coffee or tea intake should be limited to no more than two cups per day. Water intake should be at least 1.5 liter of still water a day. Remember to always eat slowly and chew well. Every meal should last at least 20 minutes.
When still on pureed foods, the patient should stick to unseasoned, caffeine-free, sugar-free, low-fat pureed products. Protein intake should be increased on week three. The patient may continue drinking protein shakes and introduce boiled or cooked eggs, jarred baby foods, pureed fish and avocados, hummus, mashed bananas, and other non-fibrous fruits.
After a month semi-solid foods may slowly be added and gradually transitioned into solid foods. Well-cooked chicken, fish and vegetables, sweet potatoes, low-fat dairy products, and low-sugar cereal are favorable choices, firstly roughly mashed with a fork. The patient should still avoid high-fat products, steaks, fibrous fruits, white potatoes, and other high-carb options. Caffeine should be reintroduced with moderation.
Note that the results of the procedure depend on one’s willingness to acquire and maintain healthy eating habits. From the fifth week forward the patient may introduce new foods and keep the emphasis on lean protein and vegetables. Sugary sweets and drinks should still be avoided. Learn to notice the difference between emotional binging and true hunger. Do not forget to keep hydrated.
Will I need to take vitamins and supplements after sleeve surgery?
Most often prescribed supplements are multivitamins with iron, vitamin D, vitamin B12, and calcium. Yearly control blood tests are advised to monitor the need for vitamins and supplements.
Send us your enquiry